Foster Care
Overview

Factors contributing to these health and developmental problems include exposure to traumatic experiences and family dysfunction, inadequate care in the family of origin, lack of prior health care, and previously undiagnosed health disorders. Traumatic experiences may include neglect, physical and sexual abuse, domestic and community violence, witnessing parents or loved ones in life-threatening situations or abusing substances, and/or family separation.
Foster care includes children and adolescents from birth to 21 years of age in court-ordered, out-of-home placement. This may involve living in a non-relative foster home, with extended family (“kinship” care), or in certain circumstances, a group home or therapeutic residential placement. [Administration: 2019]
Recognizing the unique needs of children and adolescents in foster care, the child welfare and foster care systems have expanded their roles to include responsibility for the child's overall well-being, including health, safety, stability, and permanency. Primary care clinicians can collaborate with child welfare agencies to improve the physical and mental health of children in foster care. They can leverage their unique position and relationships to engage with families of origin and foster families to minimize the trauma of separation, identify health care needs, initiate treatment, and provide health-related education. [Jones: 2020] Close surveillance and continuity of care should continue as children transition among placements.
Health Care Issues for Children and Adolescents in Foster Care and Kinship Care (AAP) assists primary care clinicians in providing trauma-informed care and meeting the health needs of children in foster care. The article emphasizes the need to seek health care early and often. [Council: 2015]
Other Names & Coding
Z13.40, Visit for screening for certain developmental disorders in childhood (standardized screening code)
Z13, Encounter for screening for other diseases and disorders
Further coding details can be found at Coding for Developmental & Mental Health Screening.
Common Behavioral and Mental Health Diagnoses
F94.2, Disinhibited social engagement disorder of childhood
F43.0, Acute stress reaction
F43.8, Other reactions to severe stress
F39, Mood disorder
F34.81, Disruptive mood dysregulation disorder (DMDD)
Z79.899, Long-term use of high-risk medication
Z02.89, Medical exam for child entering foster care
Z62.21, Child in foster care
Z63.32, Family disruption due to child in foster care or non-parental family member care
Z62.822, Parent-foster child conflict
Z62.819, History of victim of child abuse
Further coding details can be found by using the search feature at ICD10Data.com and Coding for Developmental & Mental Health Screening.
DSM-5
The Diagnostic and Statistical Manual of Mental
Disorders, Fifth Edition (DSM-5) [American: 2013] generally designates the same codes as ICD-10 does,
but its publisher, the American Psychiatric Association, prohibits including
their codes or descriptions.
Prevalence
In 2017, at least 9 out of every 1,000 children in the US suffered abuse. Of these children, 28.1% were under 3 years of age, 74.9% suffered neglect, 17.5% physical abuse, and 9.3% sexual abuse. [Child: 2019] In 2019, there were 423,997 children in foster care, roughly 1 in 202 children/adolescents. Of these children, the median age when entering foster care was 7.7 years, 44% were white, 23% Black or African American, and 21% Hispanic. [Sepulveda: 2020]
Studies have shown that 35-50% of children entering foster care have significant emotional and behavioral problems; 46% of those under age 6 have developmental problems; 80% of those under age 3 years were exposed to maternal substance abuse in utero. [Stahmer: 2005] [Ringeisen: 2008] Children and youth in foster care are more likely to have an identified special health care need and need more resources than their peers. Reported numbers of children and youth with special health care needs (CYSHCN) in foster care vary by state, comprising at least 24% of the foster care population. Some states report up to 83% as having an identified special health care need. [Sepulveda: 2020]
Genetics
Prognosis
- 47% were reunited with parent(s) or primary caretaker(s)
- 26% were adopted
- 11% went to live with a guardian
- 8% were emancipated or “aged out” of the foster care system when they became too old (usually at age 18) to receive further services
- 6% went to live with another relative
- 1% had other outcomes (includes transferal to another agency, running away, or death)
Though little data exist on long-term outcomes for children who exit foster care before 18, the effects of child abuse and neglect often have long-lasting adverse consequences for survivors. Untreated conditions, particularly emotional and behavioral ones related to traumatic experiences, are the most common reasons for foster placements to fail, which leads to further disruptions in care, school, and community for the child. [Jones: 2020] The Adverse Childhood Experiences (ACE) Study demonstrated that child abuse, neglect, and other circumstances that disrupt the child-parent relationship are significantly associated with many leading causes of adult death, such as strokes, cancer, and heart disease, and with heavy health service utilization. Stressful childhood experiences lead to higher rates of depression, suicide, cigarette smoking, diabetes, obesity, hypertension, and alcohol and substance abuse. [Felitti: 1998]
One study found that adolescents who “age out” of the foster care system suffer serious lasting consequences: 1:4 will be incarcerated within 2 years of leaving foster care; 1:5 will become homeless sometime after age 18 years; only 58% will graduate from high school (compared to the 87% national average). [Jim: 2007] Recent studies have found that adult outcomes are better when policies support youth remaining in foster care after the age of 18. [Rosenberg: 2019]
Practice Guidelines
Szilagyi MA, Rosen DS, Rubin D, Zlotnik S.
Health Care Issues for Children and Adolescents in Foster Care and Kinship Care.
Pediatrics.
2015;136(4):e1142-66.
PubMed abstract / Full Text
Keeshin B, Forkey HC, Fouras G, MacMillan HL.
Children Exposed to Maltreatment: Assessment and the Role of Psychotropic Medication.
Pediatrics.
2020.
PubMed abstract
Jones VF, Schulte EE, Waite D.
Pediatrician Guidance in Supporting Families of Children Who Are Adopted, Fostered, or in Kinship Care.
Pediatrics.
2020;146(6).
PubMed abstract
American Academy of Pediatrics, Council on Foster Care, Adoption, and Kinship Care and Committee on Early Childhood.
Health care of youth aging out of foster care.
Pediatrics.
2012;130(6):1170-3.
PubMed abstract / Full Text
Keeshin BR, Bryant BJ, Gargaro ER.
Emotional Dysregulation: A Trauma-Informed Approach.
Child Adolesc Psychiatr Clin N Am.
2021;30(2):375-387.
PubMed abstract
Kerker BD, Zhang J, Nadeem E, Stein RE, Hurlburt MS, Heneghan A, Landsverk J, McCue Horwitz S.
Adverse Childhood Experiences and Mental Health, Chronic Medical Conditions, and Development in Young Children.
Acad Pediatr.
2015;15(5):510-7.
PubMed abstract / Full Text
Roles of the Medical Home
Recommendations for adapting the medical home model for the health care needs of youth in foster care include: [Espeleta: 2020]
- Knowledge about the child welfare system and consent process in your state
- Supporting access to care and caregiver support through phone consultation
- Obtaining and maintaining updated medical records
- Implementing trauma-informed care and best practice guidelines
The primary care clinician can provide guidance about the effects of traumatic stress on development, behavior, emotions, and learning, especially during times of transition. The clinician also can provide families emotional support, validation, and tools to optimize their responses for the challenging symptoms often seen. Identifying toxic stress and related symptoms enables the clinician to advocate for the child within the child welfare system. Interventions that promote a stable foster placement and a timely, well-coordinated transition to a permanent home, including coordination of medical care, will mitigate deleterious effects on the child’s long-term development.
Toxic Stress Toolkit (AAP) (
 11.4 MB) and Parenting after Trauma: Understanding Your Child’s Needs (healthychildren.org) provide the tools clinicians will need to care for youth in foster care, identify
traumatized children, educate families about traumatic stress, and empower families
to respond to children’s behavior in ways that acknowledge past traumas but promote
more adaptive reactions to stress. Foster Care (FAQ) and Foster Care of Children with Special Needs may be helpful for foster
families.
11.4 MB) and Parenting after Trauma: Understanding Your Child’s Needs (healthychildren.org) provide the tools clinicians will need to care for youth in foster care, identify
traumatized children, educate families about traumatic stress, and empower families
to respond to children’s behavior in ways that acknowledge past traumas but promote
more adaptive reactions to stress. Foster Care (FAQ) and Foster Care of Children with Special Needs may be helpful for foster
families.
Clinical Assessment
Overview
Every child entering foster care should have a health screening evaluation before or shortly after placement. The examination should identify any safety concerns, as well as medical, mental, or dental needs that require prompt attention or that should be considered in making placement decisions. Within 1 month of the initial screen (or simultaneously with the screen), the child or adolescent should receive a comprehensive health and developmental assessment. The child’s caseworker, foster parents, and/or birth parents (if appropriate) should be present at visits and can help with acquiring medical records and history.
Consent for routine and emergency medical care, as well as the release of past medical records, should be obtained from the family or legal guardian per state regulations. Provide trauma-informed continuity of care, education and support to caregivers, follow-up care, care coordination, and child welfare system communication. [Duffee: 2021]
Comprehensive and well-child health assessments should follow Bright Futures/AAP Periodicity Schedule screening recommendations by age and risk. Follow screening guidelines for high-risk social determinates of health from Bright Futures Guidelines for Health Supervision - Pocket Guide, 4th Edition (AAP) (
 5.1 MB).
5.1 MB).The American Academy of Pediatrics has published practice guidelines for the care of children and youth in foster care based on consensus among experts due to the lack of research in this area. The guidelines provide recommendations for comprehensive medical, mental health, and dental assessments at the time of entry into foster care and ongoing coordinated care. [Szilagyi: 2015] [Council: 2015] [Duffee: 2021]
Summary of AAP Guidelines
1. Initial assessment
- Collect and update demographic information, identify the type of placement, past medical, family, and social history, and reason for out-of-home placement.
- Conduct a complete physical examination, including detailed descriptions of dermatological and other pertinent exam findings.
- Identify needs that require prompt attention, including assessment for acute injuries, chronic medical conditions, regular medications, suicide risk, and acute mental health conditions.
- Refill any medications needed before next assessment, place any urgent referrals.
- Schedule follow-up and obtain medical records.
- Identify the system of communication and care coordination with Child Welfare in your state.
- Collect comprehensive history and conduct a complete physical exam.
- Conduct age-appropriate, standardized, developmental and
trauma screening; reassess for acute injuries, chronic medical conditions,
regular medications, risk of harm to self or others, and substance use. For
all adolescents, include a HEADSS Assessment (
 72 KB)
without the caregiver in the room.
72 KB)
without the caregiver in the room.
- Identify gaps in care. Update medication list, provide medication refills as needed, update problem list and prioritize needs. Develop a care plan with dental, mental health, and specialty care referrals as indicated.
- Provide trauma-informed anticipatory guidance. Provide support and psychoeducation around the impact of adverse childhood experiences and trauma on child behavior and self-regulation. Help foster parents identify trauma triggers, set appropriate expectations, and promote trauma-informed treatment and resiliency.
- Coordinate care, including referrals, follow-up, and communication with the Child Welfare System.
- Identify team members, including social workers, mental health clinicians, school personnel, subspecialists, others as indicated.
- Continue regular return visits every 3-6 months or with placement changes.
- Ask about interval changes in social history. Youth in foster care may experience disruption in placement for different reasons. Ask about the current placement and how long the child has been living in this placement. Does the child have other siblings? If so, where are their siblings living?
- Visitations: Do they have visitations with parents and/or siblings? Are the visitations supervised? Where do they occur?
- Demographic information: Maintain updated demographic data. Include the name and contact information for the child welfare social worker (usually they are the emergency contact). Maintain the confidentiality of foster parent(s) by entering their name and contact information in the designated confidential demographic section of the health record.
Pearls & Alerts for Assessment
All children in foster care have unique health care needsLook for physical, developmental, and emotional health conditions common in children who have experienced trauma. Consider the impact of adverse childhood experiences and traumatic stress on brain development. See youth in foster care frequently, assess safety, look for gaps in care, know who can make decisions, and be aware that trauma can mimic many physical and psychiatric diagnoses. Include trauma screening, physical, dental, and developmental assessments and monitoring. Refer as needed to mental health specialists for evaluation and trauma-based treatment.
Altered responsesBiological and environmental risk factors, as well as adverse childhood experiences and traumatic stress, increase the risk for physical, developmental, behavioral, and mental health concerns. [Shonkoff: 2012] Exposed children may have problems with self-regulation (sleep disturbances, eating problems, or toileting problems) and symptoms of depression, anxiety, ADHD, aggression, self-injury, and anger that persist long after the child has been removed from the abusive or neglectful environment. Children may develop symptoms related to separation from their home and other familiar environments, which may be the most traumatic aspect of entering foster care. Primary care providers can help caregivers identify altered responses, formulate effective coping strategies, and mobilize available community resources. [Stirling: 2008]
Role as confidantMost children in foster care have been exposed to traumatic events beyond what is known or reported. Children may not be ready to discuss past trauma during the initial visit. Use positive and supportive language to build trust and support the child’s sense of self. The child may be willing to talk to their health care provider about past events, such as other physical or sexual abuse, that they have not previously disclosed. Discuss limits of confidentiality using developmentally appropriate language.
Many children in foster care have ADHD symptomsWhile set routines in a predictable home can help some symptoms, many children struggle to engage in trauma-focused mental health treatment because of inattention, impulsivity, and hyperactivity. Start with mental health screenings, including measures assessing traumatic events and trauma symptoms, refer for evidence-based, trauma-focused treatment and additional evaluation as needed in consultation with the child’s mental health therapist. [Fraser: 2019]
Monitor for suboptimal careDisruptions in care, continuity of care, and schooling can occur at the entry in foster care, during placement changes, or visits with the family of origin and can lead to increased emergency room use. [Rubin: 2004]
Reconstruct medical, medication, and immunization historyDirect contact with previous health care providers or review of previous medical records (e.g., from schools or immunization registries) may enable reconstruction of the child’s health, medication, and immunization history. The child may have been known by other names, and birthdates may be inaccurate. Verify current medications and reconcile medication lists that may be present in the electronic medical record. If immunization information is unavailable, children should be considered susceptible and immunized according to guidelines. [Szilagyi: 2015]
Screening
For Complications
-
Traumatic Stress in Pediatric Patients Care Process Model (
 ) may be used to identify the types of traumatic events a child has
experienced and related symptoms.
) may be used to identify the types of traumatic events a child has
experienced and related symptoms.
- SEEK Parent Screening Questionnaire (PSQ-R) is a free, parent screening questionnaire that targets risk factors related to child maltreatment. It is available in 4 languages and recommended for youth under 5 years.
- Comprehensive resources and screening tools are available in the Toxic Stress Toolkit (AAP) (
 11.4 MB).
11.4 MB).
 1.0 MB)
for high-risk screening guidelines.
1.0 MB)
for high-risk screening guidelines.
Presentations
Comorbid & Secondary Conditions
Common health problems of children and youth in foster care include: [Turney: 2016]
- Asthma (Asthma)
- Growth concerns
- Metabolic syndrome
- Dental caries and other dental conditions (Dental and Oral Health Screening)
- Infectious disease
- Inadequate immunizations
- Vision and hearing issues (Hearing Screening)
- Developmental delay, speech and language problems, learning disability other neurodevelopmental disabilities (e.g., Fetal Alcohol Spectrum Disorders, Autism Screening, Developmental Screening)
- Emotional dysregulation
- Sleep disturbances (Screening for Sleep Problems)
- Mental health problems
- Attachment disorder
- Post-traumatic stress disorder (PTSD)
- Depression, anxiety, and other mood disorders (Mental Health Screening for Children & Teens, Infant & Early Childhood Social-Emotional Screening)
- Behavioral disorders, such as attention-deficit/hyperactivity disorder (ADHD), oppositional-defiant disorder (ODD), and conduct disorder (CD) (Attention-Deficit/Hyperactivity Disorder (ADHD))
History & Examination
Current & Past Medical History
Family History
The foster parent or caregiver may have little or no information about the child’s family history or past social history. A young child may not use words that distinguish caregiver and family of origin relationships. Work with child welfare to obtain this information.
The foster family’s history and experience with special needs children are important in understanding how comfortable they are likely to be with managing any medical or mental health problems.
Pregnancy/Perinatal History
Developmental & Educational Progress
Maturationalprogress
Youth that identify as lesbian, gay, bisexual, transgender, and questioning (LGBTQ) are at increased risk for family relationship disruptions, discrimination, and harm. A 2019 study found that LGBTQ youth are over-represented in foster care compared to LGBTQ youth not in foster care (30.4% vs. 11.2%). These youth need protection and care that is affirming of their sexual orientation and gender identity. [Baams: 2019] [Sepulveda: 2020]
Ask about family relationships (both foster and family of origin), adjustment to foster care, peer relationships, adjustment to school, hobbies, education, or career plans. Asking caregivers about discipline techniques and assessing developmentally appropriate expectations for these very emotionally and behaviorally challenging children may help identify caregivers at risk for punishing harshly. Goals for the child’s permanent placement (e.g., reunification with parents, adoption, guardianship, or kinship placement) will guide who should be involved in health care planning and consent for treatment.
Physical Exam
General
Vital Signs
Growth Parameters
Plot growth, including BMI. Measure and plot head circumference for children less than 2 years old. Children on psychiatric medicines may experience weight loss or weight gain. Children on antipsychotic medicines are at risk for metabolic syndrome; BMI > 95th percentile or waist circumference > 90th percentile and Blood Pressure > 90th %.
Skin
HEENT/Oral
Children in foster care are at increased risk for caries and poor dental hygiene. Document any intraoral or facial injuries including bruising and frenula tears. [Pierce: 2021]
Genitalia
Testing
Sensory Testing
Laboratory Testing
- Anemia
- Lead level
- Tuberculosis (purified protein derivative tuberculin (PDD) if 3 months or older; or quantiferon -TB gold test)
- HIV
- Hepatitis B
- Hepatitis C
- Sexually transmitted infection
- Chlamydia, gonorrhea, syphilis, and HIV testing if risk assessment is positive. Follow universal screening guidelines, including HIV screening once between 15 -18 years of age. (Check state policy regarding who can give consent for testing and confidentiality of test results.) Bright Futures/AAP Periodicity Schedule
- Pregnancy testing (Check state policy regarding who can give consent for testing.)
- Evaluation for metabolic syndrome
- Fasting serum triglyceride levels (>110mg/dL)
- Fasting HDL-cholesterol (<40mg/dL)
- Fasting glucose (>110mg/dL)
- HbA1C (5.7 - 6.4 pre-diabetes; >6.5 diabetes)
- Consider maternal labs for evaluation of newborn
Imaging
Other Testing
Specialty Collaborations & Other Services
Children in foster care have a high incidence of psychiatric disorders, including PTSD. Determine if the child/adolescent was receiving mental health services prior to placement and then, if possible, coordinate ongoing care. The child welfare worker should be able to provide access to mental health assessments and treatment. Often there will be a forensic evaluation if the child or adolescent has experienced abuse. This may include a physical exam and a video-recorded interview that meets legally defined standards of care.
Preschools (see UT providers [71])
Developmental - Behavioral Pediatrics (see UT providers [9])
Early Intervention for Children with Disabilities/Delays (see UT providers [51])
Occupational Therapy (see UT providers [37])
Speech - Language Pathologists (see UT providers [65])
Psychiatry/Medication Management (see UT providers [53])
Neuropsychological Assessment (see UT providers [43])
Head Start/Early Head Start (see UT providers [26])
Treatment & Management
Overview
Because of multiple risk factors, children in foster care often benefit from the following management strategies:
- Assess safety (just because they are in custody does not mean they are safe)
- Be aware of placement disruptions, look for gaps in care and services, may need prescription refills
- Know who can make medical decisions
- Provide education and support to caregivers, continuity, tracking, and care coordination
- Symptoms of trauma can mimic many physical and psychiatric diagnoses
- Be an advocate and liaison with child welfare
Pearls & Alerts for Treatment & Management
Motivational interviewing for adolescentsMotivational interviewing can be a valuable technique for approaching risk-reduction counseling and contraception with adolescents. Motivational Interviewing (MINT) provides details of this technique.
Share the treatment planConsider the health literacy of the child and foster parents when formulating and discussing the treatment plan. Also, share the treatment plan with the child’s caseworker and birth parents if appropriate.
Balancing short- and long-term goals of careProviding primary care for children in foster care presents
several dilemmas for the clinician. First, the caregiver who accompanies the
foster child may be the foster parent, the child welfare worker, or simply a
transport provider. They may be most interested in resolving an immediate
problem (e.g., the child needs to be calmer or go to sleep) and may not
address long-term concerns or issues as most parents would. This places
greater responsibility on the primary care clinician to consider and
advocate for the child’s long-term needs and interests. Discontinuity of
care and lack of access to medical records are often a challenge since the
foster parents may prefer not to (or are unable to) continue care with the
child’s previous primary care clinician.
Multiple
psychotropic medications are often prescribed to manage behavioral symptoms.
This may be driven in part by relatively short-term goals that may not be in
the child's long-term best interest. Addressing the latter and collaborating
with foster care programs to access services that help foster families
manage symptoms non-pharmacologically may be useful.
How should common problems be managed differently in children with Foster Care?
Development (Cognitive, Motor, Language, Social-Emotional)
Prescription Medications
Systems
Other
Access to medical records
Access of individuals to protected health information is regulated under 45 CFR § 164.524. Be aware of who can have access to the medical record. Update guardian, emergency contact, and electronic access to the medical record. At the time of entry into foster care, identify the legal guardian and update electronic health record access and demographic information. Changes may need to include removing the parent’s or prior guardian’s access to the medical record. Determine if it is appropriate for the youth to have electronic access to their health record.
Confidentiality
Adolescents may be able to retain their right to confidentiality and consent for treatment for pregnancy and sexually transmitted infections. However, the current legal guardian may still have access to the medical record, including visit notes (i.e., HEADDS assessment) unless there is documentation stating that doing so may result in substantial harm. For this reason, know the related privacy rule policies for your organization.
It is appropriate to talk with the youth without the caregiver in the room to assess safety. Age-appropriate opportunities for youth to talk privately with the health care provider should be provided. Obtain consent from the caregiver and discuss the limits of confidentiality with the youth and caregiver. For example, the discussion between youth and health care provider may remain confidential unless there is a risk of harming oneself or others.
Consent
Another challenge is understanding who has legal authority to consent for care—the rules vary by state. When the state takes custody, the parents maintain legal guardianship unless the courts legally terminated parental rights. If birth parents are unavailable or uncooperative, an authorized committee or person within social services usually can provide medical consent for care. Depending on state regulations, foster parents may or may not be able to provide consent for certain medical interventions, such as medical procedures, immunizations, or medications. Primary care physicians should receive (or seek) a copy of medical consents from foster care agencies. [Strassburger: 2016]
Family
Clinicians need to understand the complexities of the child’s current living situation to support the child and the family. Become familiar with the child welfare system in your state. One-quarter of placements are likely to be in kinship care. Fifty-nine percent of children exiting foster care in 2018 returned to a parent or primary caregiver, 25% were adopted, 7% lived with other relatives (kinship care). [Children's: 2019]
Multiple studies support the benefit of kinship placements. To help these placements succeed, clinicians can help families understand the effects of adverse childhood experiences and encourage developmentally appropriate expectations and responses to the child. Lay a foundation for a child’s later understanding of foster care and self-identity by encouraging conversation using developmentally natural discussions about foster care, adoption, and birth family. Help families acknowledge racial and cultural differences. Be aware of the complexity of losses experienced by foster, adoptive, and birth parents; provide support and facilitate mental health referrals as needed. [Jones: 2020]
Caregiver Support
When parents or foster parents report significant behavioral or emotional problems with a child, consider their capacity to manage the child’s behaviors without emotional or physical abuse. Referral for respite care may be useful or, if punishment appears to be abusive, child protective services should be contacted.
Help families understand the potential for trauma-induced aberrations in bodily functions and behaviors and help determine the need for intervention. Understanding responses to trauma can help families set appropriate expectations. Toxic Stress Toolkit (AAP) (
 11.4 MB) provides useful
information to begin this educational process.
11.4 MB) provides useful
information to begin this educational process.
Mental Health/Behavior
Trauma-related toxic stress may result in neuro-dysregulation and explain behavior problems commonly observed in children that may be misidentified as ADHD, ODD, or conduct disorder. Understanding the impact of ACES and traumatic experiences on development provides a framework for caring for children and youth in foster care. See Toxic Stress Toolkit (AAP) (
 11.4 MB).
11.4 MB). In addition, agitation, anxiety, and poor attention are common responses to entering foster care and a new, unfamiliar home. Children and teens often grieve the separation from their family and feel confused by what has happened. These symptoms should be evaluated and followed to determine if they are transitory adjustments to foster care, recovery from exposure to past trauma, or a psychiatric disorder, such as ADHD or post-traumatic stress disorder..
Triggers
Family visitations will be part of the child welfare plan. Initially, the child may have no contact with their family of origin. When deemed safe, supervised visits and, depending on progress toward reunification, visits will become more frequent. Although visitation with their parents may be healing when they go well, they may bring back separation, loss, fear, and anger. It is common for children to be emotionally reactive following a visit. [Winokur: 2018] Foster families may seek guidance on managing changes in eating patterns, emotional dysregulation, and sleep following visits. For a helpful handout to guide foster families, go to Parenting after Trauma: Understanding Your Child’s Needs (healthychildren.org).
The primary care clinician may feel pressure to start or continue and monitor use of psychotropic medication(s) when they see 1) a child or adolescent as they transition from a residential setting where medicines were used, 2) a child in jeopardy of losing their foster placement or having school problems due to behavior, or 3) the caregivers and caseworkers are not able to provide an adequate past or present history.
However, psychotropic medications may not be in the child’s best interest. Disruptive behaviors, such as aggression, defiance, and temper tantrums/outbursts, may indicate a reaction to traumatic events, which does not respond well to medicine. Poor sleep may contribute to moody behavior or poor attention span. Dissociation may look like oppositional behavior or the child ignoring directions.
Take the time to involve the relevant caregivers, obtain adequate information from the homes and the school, and clarify symptoms and diagnosis.
In addition to evaluating for trauma and assessing sleep, use the “BOLDER” approach to assessment: T-MAY (Treatment of Maladaptive Aggression in Youth) Toolkit:
- Behavior: In what ways does the child exhibit aggression?
- Onset: When does it happen? What triggers it and why?
- Location: Where do the symptoms occur - home/school?
- Duration: How long does it last?
- Exacerbates: What makes it worse?
- Relief: What makes it better?
Evidence-based treatment recommendations for maladaptive aggression in youth were published in the June 2012 issue of Pediatrics. The T-MAY guidelines are as follows:
- Treatment of maladaptive aggression in youth: CERT guidelines I. Engagement, assessment, and management. [Knapp: 2012]
- Treatment of maladaptive aggression in youth: CERT guidelines II. Treatments and ongoing management. [Scotto: 2012]
- See Emotional Dysregulation: A Trauma-Informed Approach [Keeshin: 2021]
Specialty Collaborations & Other Services
Psychiatry/Medication Management (see UT providers [53])
General Counseling Services (see UT providers [298])
Neuropsychiatry/Neuropsychology (see UT providers [6])
Family Support Services (see UT providers [31])
Crisis Mental Health Care (see UT providers [25])
Address safety and address local resources, crisis numbers, apps on Mobile Devices.
Sexual Assault Counseling (see UT providers [16])
Pharmacy & Medications
-
Florida Best Practice Psychotherapeutic Medication Guidelines for Children and Adolescents (2022) (
 2.7 MB)
2.7 MB)
- GLAD-PC: Guidelines for Adolescent Depression - Primary Care (REACH Institute)
- UPOP Resources Medical Professionals
Clearly define target symptoms, expected outcomes, and potential side effects. “Start low and go slow” – one medicine at the lowest dose expected to be effective and increase dose or change/add medication deliberately to allow response both to the medication(s) and the new home environment. Follow up frequently to assess response, make needed adjustments, and provide support.
Medications do not treat oppositional-defiant disorder or conduct disorder. Refer for evidence-based treatment for trauma-related symptoms and PTSD, including Parent-Child Interaction Therapy (PCIT), trauma-informed CBT, and other evidence-based therapeutic modalities. If medication trials do not result in an expected response, consider the impact of trauma and what other behavioral and psychosocial supports need to be considered. Assess other contributing factors such as sleep disturbance, psychosocial issues, and school behavior. The use of antipsychotic medications in preschoolers (children under 6 years of age) is generally “off-label,” not recommended, and should only be considered under the most extraordinary circumstances. Disruptive aggression in autism is one such circumstance.
If considering starting a psychotropic medicine:
- Know your state’s consent guidelines for initiation of psychotropic medications. Consent guidelines may range from consent by the caregiver accompanying the child to court approval.
- Conduct comprehensive multi-informant, multi-modal, and multi-disciplinary assessments for those with a positive screen. Evaluate medical, social, and cognitive causes of behavioral symptoms. Use validated measures to assess and track psychiatric symptoms and impairment in young children, including psychosocial treatment /trauma-focused therapy.
- Assess side effects and consider laboratory tests for baseline and ongoing metabolic monitoring.
- Psychotropic medication monitoring recommendations
for youth in foster care: [Keeshin: 2020]
- Appointments every 3 months (include BMI assessment). Consider a telehealth visit if stable.
- Baseline to and periodic assessment/updates
to:
- Medical history, height, weight, BMI, waist circumference, blood pressure, heart rate, and physical and developmental assessment
- Extrapyramidal side effects (EPS)
using a validated scale, such as the Abnormal Involuntary Movement Scale (AIMS) (
 38 KB) or Extrapyramidal Symptom Rating Scale (ESRS).
38 KB) or Extrapyramidal Symptom Rating Scale (ESRS).
- Metabolic labs including fasting blood glucose or hemoglobin A1C, fasting triglycerides (repeat at 3-4 months and then annually)
- Educate families and caregivers about side effects, medication administration, maintaining an accurate medication list and bringing it to each visit, and how to make medication changes when indicated. [Keeshin: 2020]
For older children and teenagers, evaluation for depression and anxiety disorders is critical. While SSRIs are associated with increased risk of suicidal ideation, there are significant benefits in overall functioning and in decreasing actual suicide with SSRIs. Psychotherapy is the treatment of choice for a child or youth with anxiety or depression. The primary care clinician should monitor response and notify the child’s therapist of inadequate progress.
Atypical antipsychotics, such as risperidone and aripiprazole, are approved for mood stabilization in children and adolescents with bipolar disorder and symptoms of agitation and aggression associated with autism. They may decrease aggression, but the long-term side effects can be significant and demand monitoring. These medicines may provide short-term support while other services are being accessed - they should not replace intensive mental health care or be used off-label for extended periods.
Specialty Collaborations & Other Services
Psychiatry/Medication Management (see UT providers [53])
Nutrition/Growth/Bone
Specialty Collaborations & Other Services
Dieticians and Nutritionists (see UT providers [6])
Development (general)
Specialty Collaborations & Other Services
Developmental Assessments (see UT providers [54])
Developmental - Behavioral Pediatrics (see UT providers [9])
Early Intervention for Children with Disabilities/Delays (see UT providers [51])
Sleep
Specialty Collaborations & Other Services
Sleep Disorders (see UT providers [1])
Maturation/Sexual/Reproductive
Transitions
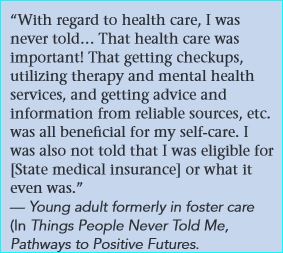
Primary caregivers can help transition patients by working collaboratively with child welfare workers and assisting youth in:
- Gathering medical records that list past health provider names, major illnesses and conditions, medications taken, immunizations, and family medical history.
- Understanding their health issues, including safe
medication use and the youth consent and assent process, and knowing
when to seek treatment. Making Healthy Choices: Guide for Youth in Foster Care on Psychotropic Medications (
 9.7 MB) may help youth understand the use, limits, and alternatives to
psychotropic medication.
9.7 MB) may help youth understand the use, limits, and alternatives to
psychotropic medication.
- Understanding why their ongoing health care should be a priority.
- Finding a new adult primary care clinician as well as needed mental health, reproductive health, and dental services. See Finding Adult Health Care.
- Understanding the importance of health insurance and working with the caseworker to identify post-foster care insurance options.
- Identify emergency contacts and other individuals who support and encourage youth to be involved in making health care decisions.
During the numerous transitions that children in foster care experience - whether during reunification with parents or primary caregivers, adoption, guardianship, or emancipation from foster care, the primary care clinician can bring a whole-child perspective of health care for these youth and work with other caregivers to ensure comprehensive health services are maintained. [American: 2012] Helping Youth Transition to Adulthood: Guidance for Foster Parents (CWIG) (
 680 KB) may be helpful for foster parents involved in transitioning youth. Other
resources include Transition Issues.
680 KB) may be helpful for foster parents involved in transitioning youth. Other
resources include Transition Issues.
Specialty Collaborations & Other Services
Mentoring Programs (see UT providers [40])
College Disability Centers (see UT providers [15])
Community & Continuing Education (see UT providers [60])
Temporary Financial Assistance (see UT providers [2])
Financial Education & Counseling (see UT providers [26])
Homeless Shelters (see UT providers [17])
Adolescent Health Transition Programs (see UT providers [5])
Dental Care Expense Assistance (see UT providers [3])
Crisis Mental Health Care (see UT providers [25])
Community Based Organizations (see UT providers [15])
Educational Advocacy (see UT providers [16])
Outpatient Mental Health Care (see UT providers [194])
Disability Rights Groups (see UT providers [25])
Ask the Specialist
What can I do to help a patient in foster care with mental health or behavioral problems?
Psychoeducation for parents, foster parents, children, and youth is powerful and reassuring. To know “I am not crazy for feeling/behaving this way” is comforting whether for the child unable to sleep due to nightmares, the youth who is agitated and can’t sit still, or the parent frustrated because the child is hoarding food or waking up in the middle of the night to access food.
Can I provide a meaningful intervention in a 15-minute visit for a patient who is depressed or traumatized?
Helping depressed adolescents: a menu of cognitive-behavioral procedures for primary care offers 7 types of basic cognitive-behavioral interventions that can be provided in a 15-minute office visit. These effective interventions build on the history taking already being done. Examples include clarifying a psychosocial problem, asking the child about their feelings surrounding it, and providing empathy. Another intervention is to coach patients on how to better present themselves so they receive the responses they really desire. This may include teaching about the impact of body posture, eye contact, speech, and tone of voice and encouraging practice techniques. Have them watch Elmo's Teaching Belly Breathing YouTube video and practice breathing exercises. Apps to Help Kids and Teens with Anxiety also may be helpful.
Resources for Clinicians
On the Web
Helping Foster and Adoptive Families Cope with Trauma: A Guide for Pediatricians (AAP) ( 3.6 MB)
3.6 MB)
Designed to strengthen clinicians' abilities to identify traumatized children, educate families about toxic stress, and empower
families to respond to children’s behavior in ways that acknowledge past traumas but promote the learning of adaptive reactions
to stress; American Academy of Pediatrics.
Child Welfare Information Gateway (HHS)
Connects child welfare and related professionals to comprehensive resources; U.S. Department of Health & Human Services.
Child Welfare Guide for Behavioral and Mental Health Professionals (Child Welfare Information Gateway) ( 288 KB)
288 KB)
Six-pages focusing on cross-system partnerships(2019).
Fostering Health Online Resource Library (NCPeds)
Best Practice documents, videos, streamlined forms for exchanging information, and information about the American Academy
of Pediatrics’ Standards of Care for the foster care population; North Carolina Pediatric Society (sign-in required).
California Evidence-Based Clearinghouse for Child Welfare
Easy access to research about screening, assessment tools, and treatment practices for children in foster care.
Council on Foster Care, Adoption, and Kinship Care (AAP)
Dedicated to improving the health and well-being of children and youth in foster care, kinship care, and those who have been
adopted.; American Academy of Pediatrics.
Learning Center for Child and Adolescent Trauma (NCTSN)
Online courses and webinars focused on child welfare issues. See particularly the 0 to 6 Child Welfare series on the left
menu; National Child Traumatic Stress Network.
National Scientific Council on the Developing Child
Information about toxic stress, the science of neglect, and much more; based at Harvard University.
Complex Trauma: Facts for Caregivers (NCTSN)
Helps parents and caregivers recognize the signs and symptoms of complex trauma and offers recommendations on how to help
children heal; National Child Traumatic Stress Network.
Improving Outcomes for Youth Transitioning Out of Foster Care (Hawai'i Kids Count) ( 2.7 MB)
2.7 MB)
Strategies to improve outcomes for youth transitioning out of foster care, such as supporting educational success, providing
employment and affordable housing opportunities, and ensuring access to health care.
How the Child Welfare System Works (Child Welfare Information Gateway) ( 789 KB)
789 KB)
Answers questions about the welfare system and what happens if abuse or neglect is reported or substantiated
Tackling Toxic Stress (Harvard University)
A series of articles that re-thinks services for children and families based on the science of early childhood development
and an understanding of the consequences of adverse early experiences and toxic stress; Center on Developing Child.
Helpful Articles
Szilagyi M.
The pediatric role in the care of children in foster and kinship care.
Pediatr Rev.
2012;33(11):496-507; quiz 508.
PubMed abstract / Full Text
Describes the purpose and problems of foster care and the primary care clinician's supporting role.
Romanelli LH, Hoagwood KE, Kaplan SJ, Kemp SP, Hartman RL, Trupin C, Soto W, Pecora PJ, LaBarrie TL, Jensen PS.
Best practices for mental health in child welfare: parent support and youth empowerment guidelines.
Child Welfare.
2009;88(1):189-212.
PubMed abstract
Summary of guidelines developed at the 2007 Best Practices for Mental Health Child Welfare Consensus Conference related to
parent engagement and youth empowerment.
Clinical Tools
Assessment Tools/Scales
M-CHAT-R/F Screen ( 1 KB)
1 KB)
Parent-completed questionnaire designed to identify children at risk of autism. An instrument available for free download
in different languages for clinical, research, and educational purposes; © 2009 Diana Robins, Deborah Fein, & Marianne Barton.
Ages and Stages Questionnaire (ASQ-3)
Parent-completed, age-specific questionnaires that screen for developmental delays in children between 1 month and 5½ years
old; available for purchase.
Ages and Stages Questionnaire: Social-Emotional (ASQ:SE-2)
A parent-completed series of 19 age-specific questionnaires screening communication, gross motor, fine motor, problem-solving,
and personal adaptive skills. Results are in a pass/fail format for domains; available for purchase.
SEEK Parent Screening Questionnaire (PSQ-R)
Parent questionnaire that screens for child maltreatment and toxic stress using 15 yes/no questions. Scroll to bottom of the
page for links to free to download in English, Chinese, Spanish, Swedish, and Vietnamese; from the University of Maryland,
School of Medicine
Department of Pediatrics.
Vanderbilt ADHD Parent Rating Scale ( 72 KB)
72 KB)
A 40-questions assessment designed to identify behavior problems and performance impairments at home; contains scoring information.
Patient Health Questionnaire (PHQ) Screeners
Free screening tools in many languages with scoring instructions to be used by clinicians to help detect mental health disorders.
Select from right menu: PHQ, PHQ-9, GAD-7, PHQ-15, PHQ-SADS, Brief PHQ, PHQ-4, PHQ-8.
SBIRT: Screening, Brief Intervention, and Referral to Treatment (SAMHSA)
Describes this evidence-based practice used to identify, reduce, and prevent problematic use, abuse, and dependence on alcohol
and illicit drugs; Substance Abuse and Mental Health Services Administration.
Children’s Impact of Event Scale-13 (CRIES-13) ( 527 KB)
527 KB)
designed for use with children aged 8 years and above who are able to read independently. It consists of 4 items measuring
Intrusion, 4 items measuring Avoidance and 5 items measuring Arousal – hence it is called the
CRIES-13.
Care Processes & Protocols
Fostering Health: Standards of Care for Children in Foster Care
Developed by an AAP multidisciplinary panel of experts, Fostering Health has been designed for use by medical, mental health,
and developmental health care professionals, as well as foster parents, social welfare agencies, members of the legal community,
health insurance agencies, and policy makers.
Standards of health care for children and adolescents in foster care are detailed in 10 chapters.
Traumatic Stress in Pediatric Patients Care Process Model ( )
)
Best-practice recommendations (2020) for the prevention of childhood trauma as well as the identification and management of
pediatric traumatic stress in primary care and children’s advocacy center settings. Includes screening and assessment tools.
Developed through a collaboration of the Department of Pediatrics at the University of Utah and the Center for Safe and Healthy
Families at Intermountain Healthcare’s Primary Children’s Hospital.
Medication Guides
Making Healthy Choices: Guide for Youth in Foster Care on Psychotropic Medications ( 9.7 MB)
9.7 MB)
Explores signs that indicate you may need help, knowing your rights and who can help, considering options, making decisions,
and maintaining treatment; 28 pages. Created by youths who have experienced foster care and the U.S. Dept. of Health and Human
Services.
Florida Best Practice Psychotherapeutic Medication Guidelines for Children and Adolescents (2022) ( 2.7 MB)
2.7 MB)
Recommendations for psychotherapeutic medication prescribing based on evidence and clinical consensus for a range of severe
behavioral health symptoms and diagnoses; Florida Center for Behavioral Health.
Psychotropic Medication Utilization Parameters for Children and Youth in Foster Care (HHS) ( 534 KB)
534 KB)
General principles, role of primary care providers, medication use criteria, and tables with dosage and schedules; Health
and Human Services (2021).
Psychotropic Medication Utilization Parameters for Children and Youth in Foster Care (Ohio Dept of Family Services) ( 437 KB)
437 KB)
Psychotropic medication practices, guidelines, ongoing monitoring, and evaluation (2014).
Toolkits
Primary Care Tools to Help Care for Children in Foster Care
Tools and resources aim to provide health care professionals with the necessary background, health assessment forms, forms
to facilitate communication and collaboration between professionals, and other materials to help care for children and teens
in foster care.
Toxic Stress Toolkit (AAP) ( 11.4 MB)
11.4 MB)
Information for primary care providers and their multidisciplinary teams serving young
children in foster care in Rhode Island but relevant for all. Includes information about the negative health impacts of childhood
adversity and toxic stress, screening tools for identifying those at highest risk for toxic stress and poor developmental
and health outcomes, and an outline of resources; American Academy of Pediatrics, Rhode Island Chapter.
GLAD-PC: Guidelines for Adolescent Depression - Primary Care (REACH Institute)
Comprehensive set of guidelines addressing issues in screening, diagnosis, and treatment of depression in adolescents age
10-21 - includes an extensive toolkit; a PDF file from Resource for Advancing Children's Health.
Health Care Toolbox
Assessment, intervention, and training tools focused on helping children and families cope with illness and injury; Center
for Pediatric Traumatic Stress at The Children's Hospital of Philadelphia.
Bright Futures in Practice: Mental Health—Volume II, Tool Kit
Comprehensive set of tools for clinicians and families; addresses mental health in various pediatric age groups; includes
a variety of resources, checklists, intake and assessment forms, and patient education materials.
Addressing Mental Health Concerns in Primary Care: A Clinician’s Toolkit (AAP)
Toolkit for pediatric care providers delivering comprehensive mental health care. Now in a new online format; available for
a fee from American Academy of Pediatrics.
Other
Four Steps to Reframing Worksheet ( 94 KB)
94 KB)
A tool for children that helps break down problems into smaller steps. Adapted from the Surviving Cancer Competently Intervention
Program – Newly Diagnosed (SCCIP-ND) manual; site developed by The Center for Pediatric Traumatic Stress and The Children’s
Hospital of Philadelphia.
Traumatic Stress in Pediatric Patients Care Process Model ( )
)
Best-practice recommendations (2020) for the prevention of childhood trauma as well as the identification and management of
pediatric traumatic stress in primary care and children’s advocacy center settings. Includes screening and assessment tools.
Developed through a collaboration of the Department of Pediatrics at the University of Utah and the Center for Safe and Healthy
Families at Intermountain Healthcare’s Primary Children’s Hospital.
Resources for Patients & Families
Understanding foster care for children with special needs, basic considerations for foster families, welcoming a child into your home, and saying goodbye to a child.
Information on the Web
HealthyChildren.org
The AAP parenting website priors foster care resources for parents, families, and caregivers.
Safe and Sound: Helping Children Who Have Experienced Trauma and Adversity
This series of resources is designed to help children who have experienced trauma and adversity, by helping their parents,
caregivers, and other adults in their lives understand how that early trauma may have affected them. Each guide can be downloaded
and shared to provide ideas for how to help children, and links to additional information and resources.
Child Welfare Information Gateway (HHS)
Connects child welfare and related professionals to comprehensive resources; U.S. Department of Health & Human Services.
Time for Reform: Aging Out and On Their Own (PEW Charitable Trusts)
Challenges of adolescents aging out of foster care systems with no permanent home or support.
Time for Reform: Preventing Youth From Aging Out On Their Own (PEW Charitable Trusts)
Recommendations for policy-level changes to enhance the success of those transitioning out of foster care.
Improving Outcomes for Youth Transitioning Out of Foster Care (Hawai'i Kids Count) ( 2.7 MB)
2.7 MB)
Strategies to improve outcomes for youth transitioning out of foster care, such as supporting educational success, providing
employment and affordable housing opportunities, and ensuring access to health care.
Helping Youth Transition to Adulthood: Guidance for Foster Parents (CWIG) ( 680 KB)
680 KB)
Discusses the critical role of foster parents, laws, and programs supporting transitioning youth; Child Welfare Information
Gateway.
The Pediatric Integrated Post-Trauma Services and Utah Psychotropic Oversight Program
The goal of PIPS is to improve the identification, health care system response, and access to treatment for children at risk
for traumatic stress. The PIPS team focuses its work in children’s advocacy centers, pediatric primary care, and foster care
settings. Includes resources for foster parents, caseworkers, and medical professionals.
National & Local Support
Foster Care Alumni of America
Connects the alumni community and works to transform policy and practice to help ensure opportunity for people in and from
foster care.
Foster Care to Success--Aging Out Institute
Nonprofit organization with resources, programs, and research to help youth age out of foster care and into independence successfully.
Studies/Registries
Foster Care (clinicaltrials.gov)
Studies looking at better understanding, diagnosing, and treating this condition; from the National Library of Medicine.
Services for Patients & Families in Utah (UT)
| Service Categories | # of providers* in: | UT | NW | Other states (3) (show) | | NM | NV | RI |
|---|---|---|---|---|---|---|---|---|
| Adolescent Health Transition Programs | 5 | 1 | 5 | 1 | 1 | |||
| College Disability Centers | 15 | 3 | 23 | 3 | 22 | |||
| Community & Continuing Education | 60 | 1 | 3 | 25 | 20 | |||
| Community Based Organizations | 15 | 11 | 18 | 18 | 50 | |||
| Crisis/Respite Care | 37 | 2 | 12 | 11 | 13 | |||
| Crisis Mental Health Care | 25 | 2 | 6 | 30 | 5 | |||
| Dental Care Expense Assistance | 3 | 2 | 2 | 5 | ||||
| Developmental Assessments | 54 | 1 | 105 | 5 | 35 | |||
| Developmental - Behavioral Pediatrics | 9 | 1 | 2 | 3 | 12 | |||
| Dieticians and Nutritionists | 6 | 1 | 1 | 4 | 3 | |||
| Disability Rights Groups | 25 | 6 | 16 | 14 | 11 | |||
| Early Intervention for Children with Disabilities/Delays | 51 | 3 | 34 | 30 | 13 | |||
| Educational Advocacy | 16 | 5 | 12 | 5 | 11 | |||
| Family Support Services | 31 | 13 | 23 | 66 | 45 | |||
| Financial Education & Counseling | 26 | 7 | 10 | 24 | 11 | |||
| Foster/Kinship Care | 25 | 2 | 7 | 13 | 13 | |||
| General Counseling Services | 298 | 1 | 10 | 213 | 30 | |||
| Head Start/Early Head Start | 26 | 10 | 66 | 18 | ||||
| Homeless Shelters | 17 | 10 | 38 | 2 | ||||
| Mentoring Programs | 40 | 1 | 3 | 20 | 9 | |||
| Neuropsychiatry/Neuropsychology | 6 | 1 | 3 | 9 | ||||
| Neuropsychological Assessment | 43 | 7 | 3 | 28 | ||||
| Occupational Therapy | 37 | 1 | 17 | 22 | 22 | |||
| Outpatient Mental Health Care | 194 | 35 | 41 | 16 | ||||
| Pediatric Dentistry | 50 | 2 | 6 | 24 | 54 | |||
| Preschools | 71 | 6 | 33 | 10 | ||||
| Prescription Drug Assistance | 39 | 19 | 20 | 38 | 23 | |||
| Psychiatry/Medication Management | 53 | 3 | 37 | 80 | ||||
| Sexual Assault Counseling | 16 | 4 | 3 | |||||
| Sleep Disorders | 1 | 2 | ||||||
| Speech - Language Pathologists | 65 | 4 | 23 | 11 | 34 | |||
| Substance Use Disorder Assessment and Testing | 43 | 1 | 18 | |||||
| Substance Use Disorder Education and Prevention | 38 | 3 | 5 | 31 | 8 | |||
| Temporary Financial Assistance | 2 | 1 | 1 | 10 | 3 | |||
| Vocational Education | 75 | 1 | 11 | 41 | 10 | |||
For services not listed above, browse our Services categories or search our database.
* number of provider listings may vary by how states categorize services, whether providers are listed by organization or individual, how services are organized in the state, and other factors; Nationwide (NW) providers are generally limited to web-based services, provider locator services, and organizations that serve children from across the nation.
Authors & Reviewers
| Authors: | Julie S. Steele, DNP, FNP-BC |
| Elizabeth R Gargaro, MD, FAAP | |
| Reviewer: | Larissa Hines, MD, FAAP |
| 2021: update: Julie S. Steele, DNP, FNP-BCA; Elizabeth R Gargaro, MD, FAAPA |
| 2014: first version: Kristina Hindert, MDA; Julie S. Steele, DNP, FNP-BCCA |
Bibliography
Administration on Children, Youth and Families, Childrens Bureau.
The AFCARS Report #26. Preliminary FY 2018 Estimates as of August 22, 2019 - No. 26.
Washington, DC: US Department of Health and Human Services; (2019)
https://www.acf.hhs.gov/cb/report/afcars-report-26. Accessed on 1/28/2020.
American Academy of Pediatrics, Council on Foster Care, Adoption, and Kinship Care and Committee on Early Childhood.
Health care of youth aging out of foster care.
Pediatrics.
2012;130(6):1170-3.
PubMed abstract / Full Text
Identifies challenges and recommendations for youth aging out of foster care.
American Psychiatric Association: DSM-5 Task Force.
Diagnostic and Statistical Manual of Mental Disorders.
Fifth ed. The American Psychiatric Publishing;
2013.
http://dsm.psychiatryonline.org/doi/book/10.1176/appi.books.9780890425...
Baams L, Wilson BDM, Russell ST.
LGBTQ Youth in Unstable Housing and Foster Care.
Pediatrics.
2019;143(3).
PubMed abstract / Full Text
Beal SJ, Greiner MV.
Children in nonparental care: health and social risks.
Pediatr Res.
2016;79(1-2):184-90.
PubMed abstract
Chasnoff IJ, Wells AM, King L.
Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure.
Pediatrics.
2015;135(2):264-70.
PubMed abstract
Chernoff R, Combs-Orme T, Risley-Curtiss C, Heisler A.
Assessing the health status of children entering foster care.
Pediatrics.
1994;93(4):594-601.
PubMed abstract
Children's Bureau: An Office of the Administration for Children and Families.
Adoption & Foster Care Statistics.
U.S. Department of Health and Human Services; (2019)
https://www.acf.hhs.gov/cb/research-data-technology/statistics-researc.... Accessed on Sept. 2021.
Child Trends.
Child maltreatment.
US Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth,
and families, Children's Bureau; (2019)
https://www.childtrends.org/indicators/child-maltreatment.
Child Welfare Information Gateway.
Foster care statistics 2013.
U.S. Dept. of Health and Human Services; (2013)
https://www.acf.hhs.gov/cb/research-data-technology/statistics-researc.... Accessed on 6/28/2021.
Report #21 available for 2013, and includes links through reports through 2019
Christian CW.
The evaluation of suspected child physical abuse.
Pediatrics.
2015;135(5):e1337-54.
PubMed abstract / Full Text
Council on Foster Care; adoption, and Kinship Care.
Health Care Issues for Children and Adolescents in Foster Care and Kinship Care.
Pediatrics.
2015;136(4):e1131-40.
PubMed abstract / Full Text
Children and adolescents who enter foster care often do so with complicated and serious medical, mental health, developmental,
oral health, and psychosocial problems rooted in their history of childhood trauma. Ideally, health care for this population
is provided in a pediatric medical home by physicians who are familiar with the sequelae of childhood trauma and adversity.
As youth with special health care needs, children and adolescents in foster care require more frequent monitoring of their
health status, and pediatricians have a critical role in ensuring the well-being of children in out-of-home care through the
provision of high-quality pediatric health services, health care coordination, and advocacy on their behalves. American Academy
of Pediatrics Policy Statement.
Duffee J, Szilagyi M, Forkey H, Kelly ET.
Trauma-Informed Care in Child Health Systems.
Pediatrics.
2021;148(2).
PubMed abstract / Full Text
Espeleta HC, Bakula DM, Sharkey CM, Reinink J, Cherry A, Lees J, Shropshire D, Mullins LL, Gillaspy SR.
Adapting Pediatric Medical Homes for Youth in Foster Care: Extensions of the American Academy of Pediatrics Guidelines.
Clin Pediatr (Phila).
2020;59(4-5):411-420.
PubMed abstract
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS.
Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood
Experiences (ACE) Study.
Am J Prev Med.
1998;14(4):245-58.
PubMed abstract
Describes the relationship between the breadth of exposure to abuse or household dysfunction during childhood and multiple
risk factors for several of the leading causes of death in adults.
Fraser JG, Noroña CR, Bartlett JD, Zhang J, Spinazzola J, Griffin JL, Montagna C, Todd M, Bodian R, Barto B.
Screening for Trauma Symptoms in Child Welfare-Involved Young Children: Findings from a Statewide Trauma-Informed Care Initiative.
J Child Adolesc Trauma.
2019;12(3):399-409.
PubMed abstract / Full Text
Jim Casey Youth Opportunity Initiative.
Time for reform: aging out and on their own.
Pew Charitable Trusts.
2007.
/ http://www.pewtrusts.org/en/research-and-analysis/reports/2007/05/01/t...
Challenges of adolescents aging out of foster care systems with no permanent home or support; Pew Charitable Trusts.
Jones VF, Schulte EE, Waite D.
Pediatrician Guidance in Supporting Families of Children Who Are Adopted, Fostered, or in Kinship Care.
Pediatrics.
2020;146(6).
PubMed abstract
Keeshin B, Forkey HC, Fouras G, MacMillan HL.
Children Exposed to Maltreatment: Assessment and the Role of Psychotropic Medication.
Pediatrics.
2020.
PubMed abstract
A clinical report that focuses on 2 key issues necessary for the care of maltreated children and adolescents in pediatric
settings: trauma-informed assessments and the role of pharmacotherapy in maltreated children and adolescents.
Keeshin BR, Bryant BJ, Gargaro ER.
Emotional Dysregulation: A Trauma-Informed Approach.
Child Adolesc Psychiatr Clin N Am.
2021;30(2):375-387.
PubMed abstract
Kerker BD, Zhang J, Nadeem E, Stein RE, Hurlburt MS, Heneghan A, Landsverk J, McCue Horwitz S.
Adverse Childhood Experiences and Mental Health, Chronic Medical Conditions, and Development in Young Children.
Acad Pediatr.
2015;15(5):510-7.
PubMed abstract / Full Text
Knapp P, Chait A, Pappadopulos E, Crystal S, Jensen PS.
Treatment of maladaptive aggression in youth: CERT guidelines I. Engagement, assessment, and management.
Pediatrics.
2012;129(6):e1562-76.
PubMed abstract / Full Text
Pierce MC, Kaczor K, Lorenz DJ, Bertocci G, Fingarson AK, Makoroff K, Berger RP, Bennett B, Magana J, Staley S, Ramaiah V,
Fortin K, Currie M, Herman BE, Herr S, Hymel KP, Jenny C, Sheehan K, Zuckerbraun N, Hickey S, Meyers G, Leventhal JM.
Validation of a Clinical Decision Rule to Predict Abuse in Young Children Based on Bruising Characteristics.
JAMA Netw Open.
2021;4(4):e215832.
PubMed abstract / Full Text
Ringeisen H, Casanueva C, Urato M, Cross T.
Special health care needs among children in the child welfare system.
Pediatrics.
2008;122(1):e232-41.
PubMed abstract
Presents levels of special health care need among children in the child welfare system and how these needs may affect children's
functioning.
Romanelli LH, Hoagwood KE, Kaplan SJ, Kemp SP, Hartman RL, Trupin C, Soto W, Pecora PJ, LaBarrie TL, Jensen PS.
Best practices for mental health in child welfare: parent support and youth empowerment guidelines.
Child Welfare.
2009;88(1):189-212.
PubMed abstract
Summary of guidelines developed at the 2007 Best Practices for Mental Health Child Welfare Consensus Conference related to
parent engagement and youth empowerment.
Rosenberg R, Abbott S.
Examining data and trends in extended foster care.
Child Trends; (2019)
https://www.childtrends.org/wp-content/uploads/2019/06/ExtendedFosterC....
Rubin DM, Alessandrini EA, Feudtner C, Localio AR, Hadley T.
Placement changes and emergency department visits in the first year of foster care.
Pediatrics.
2004;114(3):e354-60.
PubMed abstract
Evaluates the temporal relationship between Emergency Dept. visits and placement changes and underscores the need for better
health care management for foster children, particularly in the period after placement changes.
Scotto Rosato N, Correll CU, Pappadopulos E, Chait A, Crystal S, Jensen PS.
Treatment of maladaptive aggression in youth: CERT guidelines II. Treatments and ongoing management.
Pediatrics.
2012;129(6):e1577-86.
PubMed abstract / Full Text
Sepulveda K, Rosenberg R, Sunny S, Wilkins A.
Children and youth with special health care needs in foster care.
Child Trends; (2020)
https://www.childtrends.org/publications/children-youth-special-health....
Shonkoff JP, Garner AS.
The lifelong effects of early childhood adversity and toxic stress.
Pediatrics.
2012;129(1):e232-46.
PubMed abstract
Reaffirmed in 2016, this technical report presents a framework that illustrates how early experiences and environmental influences
can leave a lasting signature on the genetic predispositions that affect emerging brain architecture and long-term health.
The report also examines extensive evidence of the disruptive impacts of toxic stress.
Simms MD, Dubowitz H, Szilagyi MA.
Health care needs of children in the foster care system.
Pediatrics.
2000;106(4 Suppl):909-18.
PubMed abstract
Stahmer AC, Leslie LK, Hurlburt M, Barth RP, Webb MB, Landsverk J, Zhang J.
Developmental and behavioral needs and service use for young children in child welfare.
Pediatrics.
2005;116(4):891-900.
PubMed abstract / Full Text
Determines the level of developmental and behavioral need in young children entering child welfare (CW), estimates early intervention
services use, and examines variation in need and service use based on age and level of involvement with CW.
Stein RE, Hurlburt MS, Heneghan AM, Zhang J, Rolls-Reutz J, Silver EJ, Fisher E, Landsverk J, Horwitz SM.
Chronic conditions among children investigated by child welfare: a national sample.
Pediatrics.
2013;131(3):455-62.
PubMed abstract / Full Text
Stirling J Jr, Amaya-Jackson L, Amaya-Jackson L.
Understanding the behavioral and emotional consequences of child abuse.
Pediatrics.
2008;122(3):667-73.
PubMed abstract / Full Text
Assists caregivers by helping them recognize the abused or neglected child's altered responses, formulate more effective coping
strategies, and mobilize available community resources.
Strassburger Z.
Medical Decision Making for Youth in the Foster Care System, 49 J. Marshall L. Rev. 1103 (2016).
UIC Law Review. 2016; 49(4):53. https://repository.law.uic.edu/cgi/viewcontent.cgi?article=2706&contex...
Szilagyi M.
The pediatric role in the care of children in foster and kinship care.
Pediatr Rev.
2012;33(11):496-507; quiz 508.
PubMed abstract / Full Text
Describes the purpose and problems of foster care and the primary care clinician's supporting role.
Szilagyi MA, Rosen DS, Rubin D, Zlotnik S.
Health Care Issues for Children and Adolescents in Foster Care and Kinship Care.
Pediatrics.
2015;136(4):e1142-66.
PubMed abstract / Full Text
Turney K, Wildeman C.
Mental and Physical Health of Children in Foster Care.
Pediatrics.
2016;138(5).
PubMed abstract
Winokur M, Holtan A, Batchelder KE.
Systematic Review of Kinship Care Effects on Safety, Permanency, and Well-Being Outcomes.
Res Soc Work Pract.
2018;28(1):19-32.
PubMed abstract
Zeanah CH, Chesher T, Boris NW.
Practice Parameter for the Assessment and Treatment of Children and Adolescents With Reactive Attachment Disorder and Disinhibited
Social Engagement Disorder.
J Am Acad Child Adolesc Psychiatry.
2016;55(11):990-1003.
PubMed abstract

 Get More Help in Utah
Get More Help in Utah