Constipation
Constipation is a common problem for children with special health care needs. It can happen for different reasons and there are different ways to help. This page will talk about normal bowel function, how to prevent constipation, when to seek urgent medical attention, and tips for parents and caregivers for help with costs of laxatives and diapers.
Normal Bowel Function
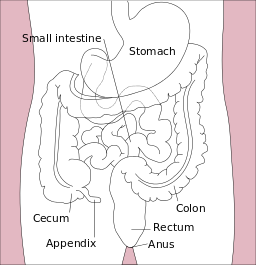
Normal bowel functions are part of the gastrointestinal (GI) system. To better understand the GI system, imagine a long tube running through the body. The parts along this tube include the mouth, esophagus, stomach, small and large intestines, and the rectal vault and anus. Food and liquid that enter the body are digested in a process that absorbs nutrients and fluids and eliminates wastes (stool, poop, or bowel movement). This system includes coordinated muscle contractions and relaxations in the walls of the GI tract. Food, stool, or gas in the GI tract stimulate this system to work by sending messages through nerve receptors that then lead to a bowel movement. This is why babies, puppies, and many mammals often have bowel movements shortly after a meal (the gastro-colic reflex).
Constipation
Babies
Toddlers and Preschoolers
School-Age Children
Prevention
You can help prevent constipation by making sure that your child gets adequate fluids and fiber in the diet, exercise, appropriate positioning, and regular, unrushed toileting time after meals. These strategies are also good first steps to treat mild constipation.
Diet
- Fluid intake—Inadequate fluid intake may contribute to constipation. Try to make sure your child drinks enough water every day. A child or teen should drink 5–8 cups of water per day; younger children should have 3–4 cups daily. Increasing water may be helpful, but can be difficult to do, particularly with a young child. Avoid using sweetened beverages, especially sodas, to increase fluid intake. 1–4 oz. per day of prune or apple juice can help with constipation in some children and infants.
- Fiber—Increasing fiber in the diet may reduce constipation. The best sources of fiber include whole grains, fruits, and vegetables. Avoiding highly processed and carbohydrate-rich foods that lack fiber may increase appetite and motivation to eat foods that are rich in fiber. If the child is tube-fed and using an enteral formula, consider switching to one with fiber.
- Stimulants—Some foods may stimulate the intestines to move more quickly. Prunes are the most common of these, but children may vary in which foods work best for them.
- Foods to avoid—Some foods can slow down digestion. Foods such as bananas, sweets, white breads, and fast food, foods that are high in fat, and large amounts of dairy products all tend to slow digestion and contribute to constipation. This varies among children.
- Refer to a nutritionist as needed (Dieticians and Nutritionists (see UT providers [6]).)
Habits
- Meals—Regular meals are helpful in keeping the bowels moving. Timing opportunities to use the toilet to follow meals can enhance the ease of passing bowel movements.
- Less snacks—Snacking, particularly “grazing” (eating small amounts of food, usually low in fiber, throughout the day), can limit the amount of food eaten at meal times and result in a poor gastro-colic reflex, resulting in poor gut motility and constipation.
- Exercise—Kids who get plenty of exercise seem less likely to get constipated. Assuring daily exercise has other benefits in terms of fitness and weight control.
- Behavioral issues—Positively reinforce all passage of stool. For children who are toilet trained, ensure adequate time and privacy for defecation (e.g., it isn’t going to happen in a public school bathroom stall). Treat accidents with a neutral approach.
- Toileting routine—It is helpful if your child goes to the toilet and tries to poop after meals. This is particularly important after breakfast on school days, when he or she may not have another opportunity to poop till evening. See Toilet Training Children with Complex Medical Conditions
- Positioning—Ensure child is adequately supported in an upright position to allow optimal defecation. For children with mobility issues, time in a stander or at a standing table may help with evacuation. An adapted toilet seat may be necessary for proper positioning. Speak with your child’s physical therapist or primary care physician about the best options and how to obtain this equipment through insurance or Medicaid.
- Warm baths—A warm bath once a day can help to relax the muscles of the rectum and make it easier for your child to have a bowel movement.
Treatment
Maintenance Therapy
When to Seek Urgent Medical Attention
- Pain doesn’t go away or is getting worse
- Blood is in or around the stool (can be non-urgent, but check with your physician if this is new)
- Swollen, firm abdomen that is painful to the touch (seek immediate medical attention) or associated with fever
- Vomiting or dehydration related to the constipation or bowel problem
- Stool is not able to be passed despite interventions
- An enema has not come back out
Tips for Parents and Caregivers
Lowering Your Out-of-pocket Cost for Laxatives
Help with Diaper Costs
Resources
Information & Support
For Parents and Patients
About Kids GI Health (IFFGD)
Reliable digestive health knowledge, support, and assistance about functional gastrointestinal and motility disorders in children
and adults; International Foundation for Functional Gastrointestinal Disorders.
Constipation in Children (AAP)
Learn how to know if your child is constipated and, if so, what to do about it; on HealthyChildren.org, sponsored by the American
Academy of Pediatrics.
Kids Need Fiber: Here’s Why and How (AAP)
Printable website with information about fiber and reading nutrition labels to help prevent constipation and other health
problems; HealthyChildren.org.
Dietary Fiber (IFFGD)
Information about different kinds of fiber, how to incorporate fiber into the diet gradually, and serving sizes to help prevent
constipation; International Foundation for Functional Gastrointestinal Disorders.
Let's Talk About... Constipation in a Child: Bowel Clean Out (Spanish & English)
Guide for caregivers on bowel clean-out and daily care for constipation at home; Intermountain Healthcare.
UCanPoopToo Program (BeHealth Solutions)
Online program that provides education and ongoing tools to solve the physical, emotional and behavioral issues of encopresis.
Services for Patients & Families in Utah (UT)
| Service Categories | # of providers* in: | UT | NW | Other states (3) (show) | | NM | NV | RI |
|---|---|---|---|---|---|---|---|---|
| Clothing Assistance | 79 | 2 | 33 | 2 | ||||
| Dieticians and Nutritionists | 6 | 1 | 1 | 4 | 3 | |||
| Prescription Drug Assistance | 39 | 19 | 20 | 38 | 23 | |||
For services not listed above, browse our Services categories or search our database.
* number of provider listings may vary by how states categorize services, whether providers are listed by organization or individual, how services are organized in the state, and other factors; Nationwide (NW) providers are generally limited to web-based services, provider locator services, and organizations that serve children from across the nation.
Authors & Reviewers
| Authors: | Tina Persels |
| Jennifer Goldman, MD, MRP, FAAP |

 Get More Help in Utah
Get More Help in Utah